Posted by: Metrolina Eye Associates in Floater, Uncategorized
WHAT ARE FLASHES AND FLOATERS?
Flashes and floaters are common ocular symptoms that can range from a large floater across the vision (sometimes mistaken for a “piece of dirt” on one’s glasses) to episodes of photopsias (small flashing white lights in the peripheral field of vision). Moreover, a patient can experience “thousands” of small floaters coming down through the field of vision. The question that arises is, do these symptoms indicate that an urgent ophthalmology assessment is required? Should this patient wait for a regular follow-up appointment or be advised to seek ophthalmic care immediately? The answer is almost always that this patient should be seen in a timely manner and you can see why below.
WHO GETS FLASHES AND FLOATERS?
Most cases of acute onset monocular floaters and/or flashes, unassociated with other symptoms, are ocular in nature and are due to posterior vitreous detachment (PVD). Uncomplicated floaters and flashes typically represent PVD, which is an age-related event. The reported prevalence of PVD increases from 24% in adults aged 50 to 59 years, 37% amongst those 60-69 years, 59% amongst those 70 to 79 years, to 87% amongst 80 to 89 years. The prevalence of PVD also increases with the presence of myopia, trauma, and intraocular inflammation. While most people will develop PVD at some point in their lives, it is often asymptomatic and in the majority of cases a benign occurrence without any long-term complications. However, 10-30% of individuals who present to an eye care professional with acute symptoms have a full-thickness tear or hole in the retina; this complication of PVD can lead to retinal detachment and permanent visual loss in 33-46% of cases if left untreated. While floaters and/or flashes are common, retinal detachment is uncommon with an estimated incidence of 0.8-1.8/10,000 persons per year and prevalence of 0.3%. Prompt diagnosis and surgical treatment can restore vision and prevent impending vision loss in those patients.
POSTERIOR VITREOUS DETACHMENT (PVD)
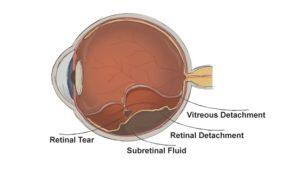
Posterior vitreous detachment (PVD) involves separation of the posterior vitreous from the retina as a result of vitreous degeneration and shrinkage that produces floaters and/or flashes.
Figure : Diagram of the human eye. Posterior vitreous detachment is shown. There is an associated retinal detachment with subretinal fluid between the neurosensory retina and the retinal pigment epithelium.
Floaters are a sensation of gray or dark spots moving in one’s visual field and they are caused either by light bending at the interface of fluid pockets in the vitreous jelly or cells located within the vitreous. This symptom involves one or more monocular “cobwebs” within or near the central vision that blurs but does not eliminate sight. Flashes of light are caused by traction forces on areas of the peripheral retina applied by the tightly adherent vitreous jelly. Patients typically describe monocular, repeated, brief flashes of white light that occur in their peripheral visual field.
Figure: Artist representation of floaters as viewed from the patient.
Retinal detachment occurs when the neurosensory layer of the retina separates from the underlying retinal pigment epithelium disrupting the photoreceptors and eventually precipitating tissue necrosis if untreated. In the majority of cases fluid gains entry to the subretinal space through a full-thickness retinal tear or hole as a result of traction on the retina from PVD. The decrease in visual acuity associated with a retinal detachment is typically due to secondary vitreous hemorrhage, significant vitreous debris, or detachment of the central retina. Such symptoms may create a progressive monocular visual field defect (‘curtain of darkness’).
WHAT DOES THE LITERATURE RECOMMEND?
I am a vitreoretinal subspecialist and in 2009, we published a study entitled, Acute-Onset Floaters and Flashes: Is This Patient at Risk for Retinal Detachment? in the Journal of the American Medical Association (JAMA) to determine the accuracy of historical features and physical examination in the diagnosis of retinal tears in patients presenting with floaters and/or flashes.
We reviewed the 17 best studies in our final analysis and found that the probability of retinal tear amongst patients bothered enough by floaters and/or flashes is around 14%. In patients with acute symptoms, subjective visual reduction is the most important finding for retinal tears. In addition, the presence of vitreous hemorrhage or vitreous pigment are the most predictive signs for retinal tear. Patients initially diagnosed with an uncomplicated PVD carry a 3.4% chance of a future retinal tear within 6 weeks. During those 6 weeks, the new onset of more than 10 floaters or the new onset of subjective visual reduction identify high-risk patients.
THE BOTTOM LINE
The acute onset of floaters and/or flashes is common in older adults and posterior vitreous detachment is the usual ocular cause. Although posterior vitreous detachment is usually a benign occurrence, sight-threatening complications including retinal tears and retinal detachments can occur. Among patients bothered enough by floaters and/or flashes from ocular causes that they get an ophthalmology assessment, most have posterior vitreous detachments and around 14% may have a retinal tear.
WHAT SHOULD YOU DO?
If you experience bothersome flashes or floaters, contact your Metrolina eye physician and we will arrange for you to be evaluated. You can expect a dilated examination to look for posterior vitreous detachment and rule out retinal tears or detachment. If you have any questions, please feel free to contact us any time.
By David Almeida, MD, MBA, PhD