Age-Related Macular Degeneration (AMD)
What is AMD?
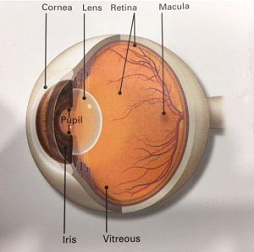
Age-Related Macular Degeneration (AMD) is a problem with your central retina. It happens when the central part of the retina called the macula is damaged. With AMD you lose your central vision. You lose the ability to see fine details, whether you are looking at something close or far. AMD is a leading cause of vision loss in older adults above 50 years of age.
Two types of AMD
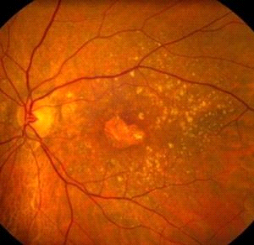
Dry AMD: This form is quite common. About 80% -90% (8 out of 10) of people who have AMD have the dry form. Dry AMD is when parts of the macula get thinner with age and tiny clumps of protein called drusen grow. You slowly lose central vision. There is no way to treat dry AMD yet.
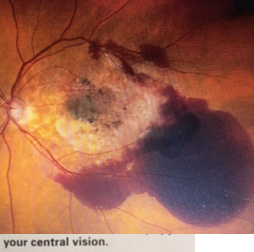
Wet AMD: This form is less common but much more serious. Wet AMD is when new, abnormal blood vessels grow under the central retina, the macula. These vessels may leak blood or other fluids, causing scarring of the macula. You lose vision faster with Wet AMD than with dry AMD. Over 90% of Wet AMD patients suffer significant visual loss within 2 years if left untreated. Discuss with your retina specialist about treatment options.
Many people don’t realize they have AMD until their vision is very blurry. Therefore, it is important to have regular visits to an ophthalmologist. Your Physician can look for early signs of AMD before you have any vision problems.
Symptoms to look for
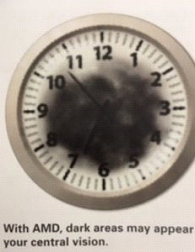
In macular degeneration, patients suffer varying degrees of destruction to the retina tissue and can experience a wide spectrum of visual problems. These include, but are not limited to:
However, even patients with advanced macular disease tend to retain excellent peripheral vision.
How is AMD diagnosed?
During an eye exam, your ophthalmologist will dilate your pupil and look through a special lens at the inside of your eye. Your doctor may do fluorescein angiography to see what is happening with your retia. Yellow dye (called fluorescein) is injected into a vein, usually in your arm. The dye travels through the blood vessels. A special camera takes photos of the back of your eye as the dye travels throughout its blood vessels. This shows if abnormal new blood vessels are growing under the retina.
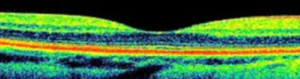
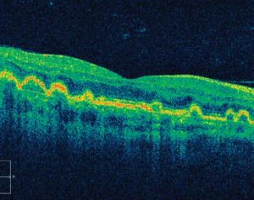
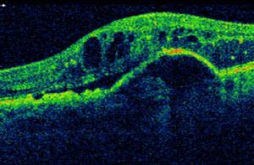
Optical coherence tomography (OCT) is another way to look closely at the retina. A machine scans the retina and provides very detailed images of the retina and macula.
Picture of Wet Macular Degeneration below:
Picture of Dry Macular Degeneration below:
Optical coherence tomography (OCT)
OCT is a newer, non-invasive, quick exam that has gained universal acceptance during the last decade and is now used by many ophthalmologists to visualize the retinal microarchitecture. See images below.
Normal OCT
Dry AMD OCT
Wet AMD OCT
How is AMD treated?
Dry AMD
Right now, there is no way to treat the dry form of AMD. However, people with lots of drusen or serious vision loss might benefit from taking a certain combination of nutritional supplements. A large study found those people may slow their dry AMD by taking these vitamins and minerals daily:
Your ophthalmologist can tell you if vitamins and minerals are recommended for your dry AMD.
Wet AMD
To help treat wet AMD, there are medications called anti-VEGF drugs. VEGF causes growth of “leaky” blood vessels in wet macular degeneration. Anti-VEGF treatment helps reduce the size and leakage of the abnormal growing blood vessels under the macula.. These medications include Avastin, Lucentis, and Eylea. This medicine is delivered to your eye through a very slender and short needle. While the thought of an “eye shot” might cause many to cringe, in our experience, there is little, if any, patient discomfort, and the spectacular visual gains far outweigh any fears.
In contrast to prior therapies, these medications have improved vision for many patients with wet macular degeneration. Several large national and international studies have shown that Avastin, Lucentis, and Eylea all work well. Your retina specialist will discuss which medication may be best suited for your situation.
In general, repeated injections are the norm to keep the fluid from recurring. Frontiers in treatment of wet AMD include finding medications that may even better restore vision and prolong the interval between injections.
While medications that block VEGF have received much media attention and deserved fanfare for their impact on wet AMD, invaluable work continues in the dry AMD front as well. Many vitamin therapies are already available to slow the progression of dry AMD.
Laser surgery may also be used to treat some types of wet AMD. Your eye surgeon shines a laser light beam on the abnormal blood vessels. This reduces the number of vessels and slows their leaking. As a general rule, patients who receive treatment in a timelier fashion tend to fare better than those who delay evaluation by a retina specialist.
Test your vision with the Amsler Grid
Every patient diagnosed with macular degeneration should establish a daily routine for monitoring their own vision. You may notice these changes when they happen. But you may catch vision changes as soon as possible. Treating them early can help slow or stop further loss of sight. You should use an Amsler grid every day to monitor your vision.
Normal Amsler Grid below:
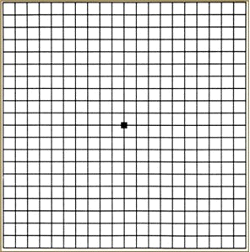
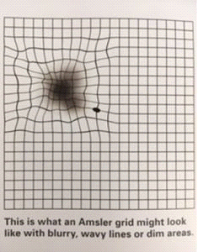
This is what an Amsler grid might look like with blurry, wavy lines or dim areas.
Making the most of the vision you have
If you have AMD, you can learn how to make the most of your vision. Often you can still do many of your favorite things with special low vision tools. These can include different kinds of magnifying tools, handheld computers, electronic items and more.
Also, you can learn how to use your side vision to help you do things. A vision rehabilitation specialist can teach you how this works. They also can help you find many low vision support services and tools.
Ask your Ophthalmologist to help you find a vision rehabiliation specialist in your area. The goal is to learn new ways to be as independent as possible.
