Retinal Detachment
What is a retinal detachment?
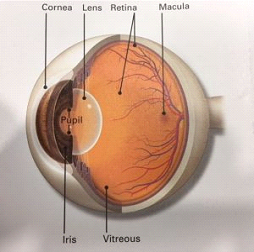
The retina is the inner lining of the back of the eye. A retinal detachment is when the retina lifts away/off from its underlying surface known as the retina pigment epithelium. The retina does not work when it is detached and is a serious sight threatening problem. An Ophthalmologist needs to diagnose this right away, otherwise you can lose sight.
How do you get a detached retina?
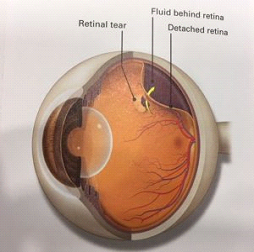
As we age the vitreous (the jelly like substance that fills the middle of the eye) begins to shrink and break down into a liquid. The Jelly is attached to the retina at certain points and when the eye moves the vitreous does to, and subsequently releases from the retina. During the process of vitreous releasing from the retina the vitreous may be too adherent to the retina thus yanking a piece of retina with it as it attempts to release from it. As a retinal break develops it allows fluid from inside the eye to seep underneath the retina subsequently leading to a retinal detachment.
Who is at risk for a detached retina?
You are more likely to have a detached retina if you:
Symptoms of a detached retina
How is a detached retina diagnosed?
Your Ophthalmologist will dilate your pupil with eye drops. Then they will look through it with a special lens to check your retina.
How is a detached retina treated?
Surgery is done to repair a detached retina. There are several types of detached retina surgery:
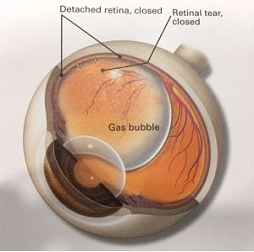
Pneumatic retinopexy is usually an office-based procedure using laser or freezing therapy to seal off a tear, followed by injecting a small gas bubble into the eye to reattach the retina from inside the eye. The gas bubble pushes the retina into place so it can heal properly. This requires special positioning for a few days directed by the physician. The positioning keeps the bubble in the right place. Over time the bubble is absorbed. The bubble may take one to six weeks to absorb completely depending on the gas used.
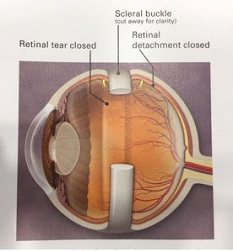
Scleral buckle surgery is conducted in the operating room. A band of rubber or soft plastic or sponge is sewn to the outside of the eyeball. It gently presses the eye inward. The buckle helps the detached retina heal against the eye wall. A buckle is generally not visible after the eye has healed.
Vitrectomy surgery is also an operating room procedure that is used by itself or can be combined with a scleral buckle. A small cutting instrument is used to enter the eye through a 1 mm incision, and the vitreous gel is removed and replaced with a gas bubble or silicone oil. If an oil bubble is used the oil will be removed a few months later in the operating room. With an air or gas bubble, you cannot fly in an airplane or travel to high altitudes because it may cause the gas to expand, which will increase the eye pressure. You may fly safely with a silicone oil bubble. You will need to keep your head in a very specific position as your doctor recommends. Vitrectomy surgery is now more commonly used to treat retinal detachment induced by a retinal tear.
Vitrectomy, scleral buckle and gas are sometimes used in combination. Anatomical success rate can be as high as 80 – 90 percent. However, some eyes will develop recurrent retinal detachment and may need additional surgery.
Surgery is generally performed as an outpatient procedure, and patients may go home the same day.
What are the risks of surgery for detached retina?
What to expect after surgery:
Healing time varies from several weeks to months depending on the extent of surgery. You may have some pain for a few hours and soreness for several weeks afterwards. You will be given pain medication.
Expect the eye to be puffy and red for several days with clear, reddish tears and discharge. Cold packs on the closed eyelids help the swelling go down and provide comfort.
Rest and less activity is advised after surgery for a few weeks as you perform the positioning exercises instructed if a bubble is put in your eye.
You may notice the bubble in your eye and you might see floaters and flashes for a few weeks.
Your sight should begin to improve about 4 weeks after surgery. It could take months after surgery for your vision to stop changing. Plus, your retina may still be healing for a year or more after surgery.
If the center part of the retina (macula) has been detached, the central (reading) vision may not completely return.
You may experience nausea immediately after the surgery. Please tell your doctor so that anti-nausea medication can be prescribed.
Your doctor will instruct you about postoperative eye drops and activities. Generally, allow at least one month before returning to full physical activity. As noted above, always check with your doctor to determine if it is safe to resume air travel.
Your eye power may change after the surgery. Glasses or contact lenses are prescribed 6 to 8 weeks after successful healing.
Please contact us immediately during the postoperative period if you experience the following symptoms:
